Interesting Radiology Cases
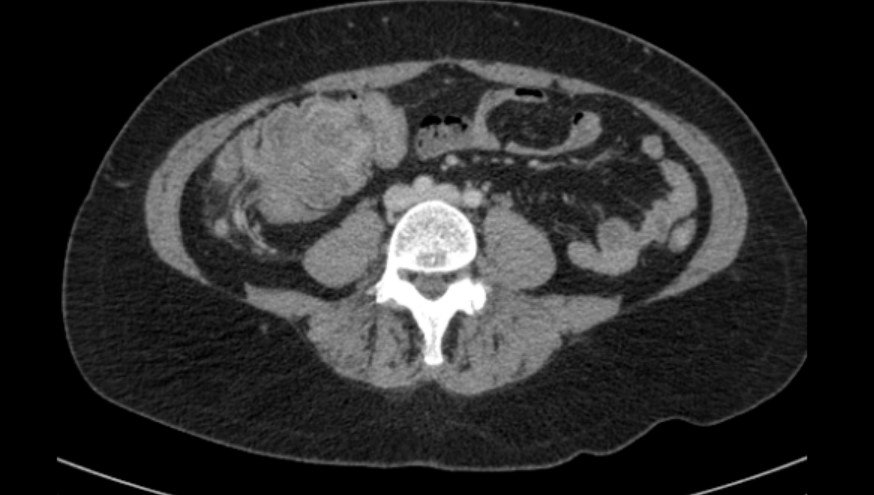
RADIATION ENTERITIS
This is a middle-aged patient who had presented 6 months after hysterectomy due to endometrial malignancy. A CT scan revealed extensive mucosal hyperenhancement, mural thickening and perienteric fat stranding of the small bowel loops below the level of the pelvic brim. The loops of bowel above the pelvic brim appear to be normal. On close questioning it was revealed the patient had long course of radiotherapy to the pelvis for lymphadenopathy. The case is a classical example of radiation enteritis in the radiation field below the pelvic brim.
The radiation also has caused a degree of stricture of the right vesicoureteric junction causing hydronephrosis on the right side.
PANCOLITIS
This is a patient who had presented with bloody diarrhoea after a recent episode of chest infection. A CT scan demonstrated extensive mucosal hyperenhancement, mural thickening and pericolic fat stranding extending from the caecum to the rectosigmoid junction. Appearances in keeping with PANCOLITIS. The differentials for this include inflammatory bowel disease and C. difficile colitis. This is unlikely to be ischaemic colitis as there is overlap of SMA and IMA territory. On close questioning, patient revealed recent treatment for chest infection- pneumonia with intravenous Augmentin. As evident on the CT scan, there is left basal consolidation with left-sided pleural effusion. C. difficile pancolitis is due to the broad spectrum antibiotic administration. This happens is a complication more so in elderly patients.
ILEOCOLIC INTUSUSCEPTION
CT abdomen and pelvis: The patient presented with acute onset abdominal pain lasting for a few hours with history of recent diarrhoea and change in bowel habits. The CT scan demonstrates a polypoidal lesion in the proximal colon measuring approximately 2 cm which acts as a lead point. This causes ileocolic intussusception. This is a serious condition in which part of the intestine slides into an adjacent part of the intestine. The telescoping action often blocks food or fluid from passing through. There are surrounding nodular lymph nodes in the ileocolic branch of the right lower quadrant likely due to local infiltration. There is hyper-enhancing mucosa and mural oedema causing a degree of congestion. The lesion is likely to be malignant as there are features of liver metastasis in the segment 7 and segment 8.
SITUS AMBIGUOUS CHOLECYSTITIS
CT abdomen and pelvis: The patient presented with left-sided upper quadrant pain. Clinical examination revealed mass like pathology in the left upper quadrant.
CT scan demonstrates a left sided liver with 2 normal appearing spleens on the right side. Numerous surrounding splenenculi noted. There is evidence of abnormal gallbladder with mucosal hyperenhancement, mural thickening and pericholecystic fat. Features in keeping with acute cholecystitis. The IVC continues as the azygos vein and enters the right atrium from the cranial side. The heart and great vessels appear orthotopic. The lungs demonstrate bilateral isomerism with no evidence of middle lobe. The fluid is noted in the rectovesical pouch.
BILIARY HAMARTOMATOSIS
MRI study: This patient presented with abnormal liver function tests. Ultrasound had demonstrated numerous cystic lesions throughout the liver. Further evaluation with contrast-enhanced MR scan was performed. There is evidence of extensive cystic lesions throughout the liver parenchyma which appear to be communicating to the biliary radicals. No evidence of restricted diffusion or signal dropout on ADC. Postcontrast there was no evidence of enhancement or presence of any solid lesions. Appearances are in keeping with biliary hamartoma. The differential for this is polycystic disease. Since the kidneys are not affected, this would be unlikely. Final diagnosis was biliary hamartomatosis.
MRCP-CBD CALCULUS
MRCP: Patient had presented with extreme degree of jaundice and right upper quadrant pain. Ultrasound initially had demonstrated dilated biliary radicles. MRCP was carried out. In this case we can visualise extensively dilated intra and extrahepatic biliary dilatation. A large filling defect measuring 11 mm is noted in the CBD. The pancreatic duct is not dilated. There are 2 separate calculi, one in the ampulla and the other in the mid CBD causing significant obstruction and dilatation of the biliary tree and the gallbladder. Patient proceeded for ERCP.
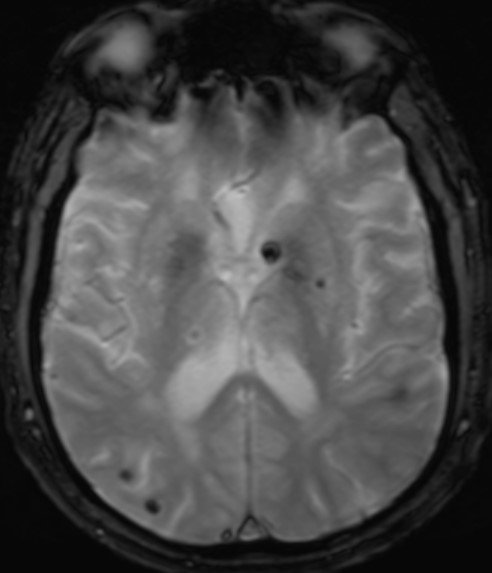
AMYLOID ANGIOPATHY AND ACUTE HEMORRHAGE
MRI brain: Patient presents with recurrent headache and transient ischaemic attacks. However he had no focal neurology. On one occasion he had severe headache. MRI scan demonstrated numerous foci of petechial haemorrhage and lacunar haemorrhages evident on gradient echo sequences. A large focus of acute haemorrhage in the right parietal cortex is also noted. Postcontrast there was normal appearing circle of Willis including the carotid and vertebrobasilar systems Numerous haemorrhagic foci also noted in the posterior fossa as well.
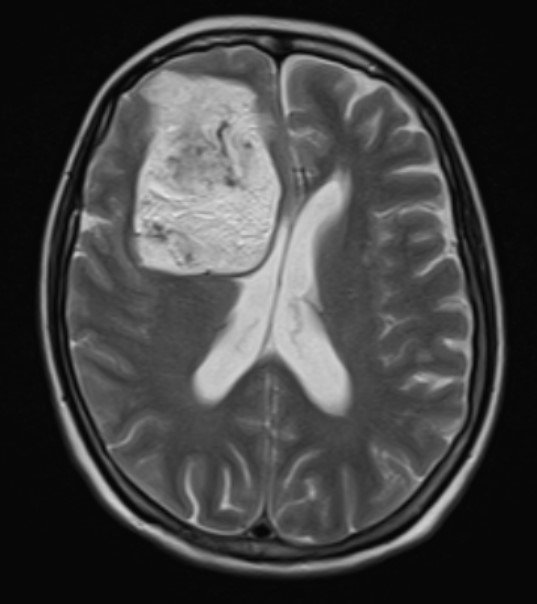
MRI BRAIN DERMOID
MRI brain: Patient presented with unilateral headache. MRI demonstrated a large heterogeneous mass lesion in the right frontal parietal cortex with foci of haemorrhage. Postcontrast there was heterogenous enhancement. Appears to be closely related to the wing of the sphenoid. Normal appearances of the left cortex and the posterior fossa. Features are consistent with heterogeneously enhancing dermoid cyst. Differential for this includes partially thrombosed large aneurysm of the right ICA.
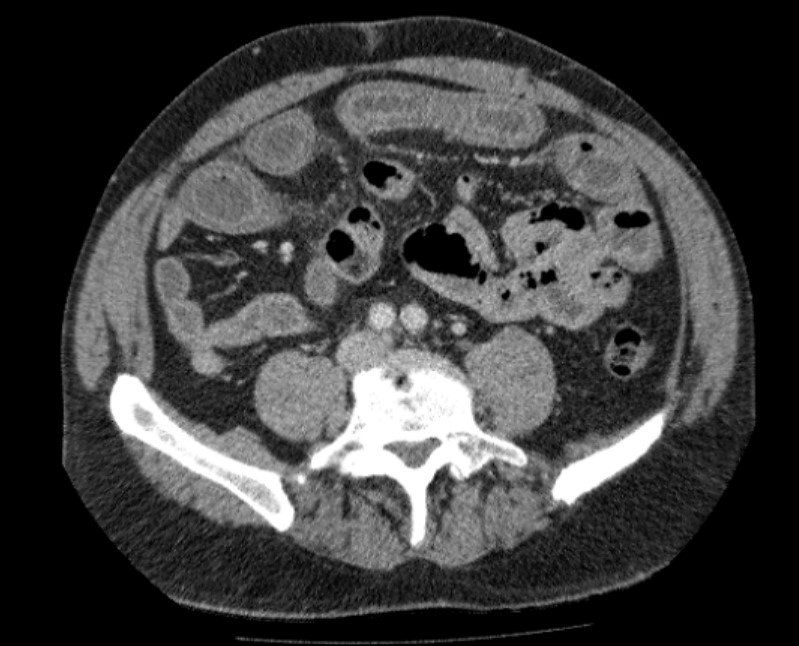
PRIMARY PERITONEAL CAKING WITH DIFFERENTIALS
CT abdomen and pelvis: Patient presented with abdominal discomfort and recent weight loss. CT of the abdomen demonstrated extensive peritoneal infiltration and omental caking. Free fluid also noted in the peritoneal cavity including the pouch of Douglas. The bowel loops are patent with no evidence of obstruction. Some free fluid also noted around the liver and spleen tracking along the paracolic gutters. Features are in keeping with primary peritoneal malignancy with extensive infiltration. The differentials for this could be ovarian malignancy, but the ovaries appear to be preserved. The other differential possibly could be disseminated tuberculous peritonitis.
EMPHYSEMATOUS CHLOLECYSTITIS & OPEN LOOP LARGE BOWEL OBSTRUCTION
CT abdomen and pelvis: Patient presented with right upper quadrant pain and vomiting. CT scan demonstrated extensive intramural air in the gallbladder with emphysematous cholecystitis. Air is also noted in the CBD.
In addition there is evidence of bowel obstruction with dilated loops of small bowel measuring up to 33 mm. The cause of obstruction is due to the adhesions / sepsis and dilatation of ascending colon and consequently small bowel dilatation due to incompetent ileocecal valve. There is evidence of previous anterior resection. Patient was noted have uncontrolled diabetes causing the emphysematous cholecystitis.
CT ABDOMEN WITH CROHNS DISEASE
The patient presented with abdominal pain and weight loss. The CT scan demonstrated inflammatory bowel disease with the distal ileum and the terminal ileum demonstrating mucosal hyperenhancement, mural thickening and perienteric fat stranding. There was lack of peristalsis indicating hose pipe appearance. There was no evidence of desmoplastic reaction or phlegmon formation. Large bowel was grossly normal. No perforation or obstruction. Features were in keeping with uncomplicated Crohn’s disease of the distal and terminal ileum.
CT BRAIN WITH RING ENHANCING LESIONS
CT Brain: Patient presented with fever and headache. CT scan demonstrated multiple foci of hypodense lesions with surrounding versus any remarkable. Postcontrast there is evidence of ring enhancement. The differential for this include a ring-enhancing metastatic deposits and ring-enhancing septic emboli. Since the patient was septic these were considered to be septic emboli causing abscess. Further evaluation demonstrated endocarditis on echocardiography.
contact us &
Get started with our premium diagnostic services today!